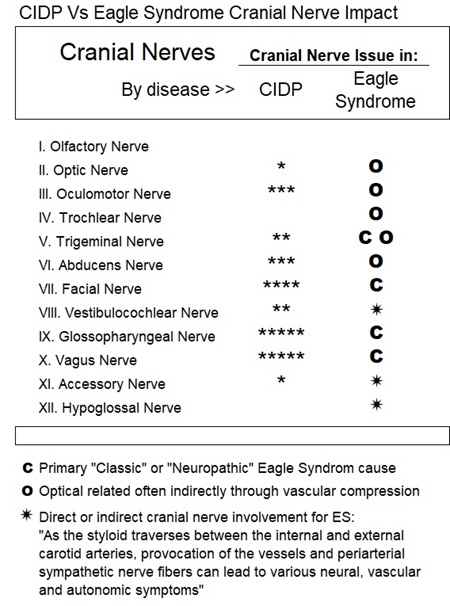
My CIDP log of CIDP versus Eagle Syndrome 2024 and onward: Some CIDP Symptoms may actually be caused or triggered by an elongated styloid process - a bone / ligament structure between my right ear and chin. Eagle Syndrome versus CIDP : cranial nerves + parasympathetic and sympathetic?:
July 16, 2024 Eagle Syndrome Diagnosis by a Dental Surgeon: a potential breakthrough on eye / facial pain as I have a diagnosis of "Eagle Syndrome", believe it or not after referral by my dentist! I had previously seen more than a handful of doctors and came up with a highly questionable diagnosis, a blank, or denial that anything was wrong. This included two visits to hospital emergency 2021 and discussions with my cidp neurologist and her referrals. Eagle Syndrome, caused by an elongated styloid process and/or calcified stylohyoid ligaments, could explain pretty much all my eye/ head/ face issues as it effects the carotid arteries, jugular vein and cranial nerves. See Dental Surgeon panoramic x-ray showing my elongated styloid process. Symptoms associated with Eagle Syndrome are due to impingement of adjacent anatomical structures contained within the carotid sheath including the carotid artery, jugular vein, glossopharyngeal nerve and vagus nerve, cranial nerves 9 and 10 respectively*. The vagus is the longest nerve of the autonomic nervous system in the human body and comprises both sensory and motor fibers: It contributes to the autonomic nervous system, which consists of the parasympathetic and sympathetic parts. However, about 15% of CIDP patients overall have cranial nerve and bulbar involvement also - and my version of the CIDP, MADSAM category, almost 50% involvement†. Eagle Syndrome is neuropathic and neurological. Eagle Syndrome can be dangerous causing frequent syncope (for example), even life-threatening via bilateral carotid artery dissection or stroke††
v BIG QUESTION: Does Eagle Syndrome / Stylohyoid Syndrome cause or trigger my eyeball fasciculations, fasciculations generally, mini-seizures, "mind-blackouts" (march 2022), arrhythmia, and most of my facial pain. And what about the really weird spontaneous jaw-snapping I logged on January 12, 2021, Could Eagle Syndrome even be responsible for my mid-2013 unsettling breathing problems and near-death breathing crisis January 17, 2023 that I attributed to CIDP? -
Summary Log Living with both CIDP and Eagle Syndrome - an Astonishing diagnosis by a Dental Surgeon July 16, 2024 -
CIDP Chronic Inflammatory Demyelinating Polyneuropathy Vs. Eagle Syndrome / Stylohoid Syndrome
v My CIDP 2024 with astonishing diagnosis of Eagle Syndrome / Stylohyoid Syndrome / Stylalgia: » March 06, 2024: Off all CIDP related drugs for a third year since February 11, 2021; only taking 75 mg/day of Metoprolol for arrhythmia. My top ranked CIDP symptom is facial fasciculations, facial pain and dry mouth. My eyes "bubble like boiling water", especially when closed to sleep, as typical with other bodily CIDP fasciculations. I have found wearing a hoody at night the best solution and now I am able to manage the situation.
»March 06, 2024: I have no diagnosis for my facial pain but I am starting to wonder if the immunoglobulin IgG infusions I took for a decade is a factor. I think this because I had facial, neck and lips sores every time I infused. Could I have adhesions from tissue repair that interfered with my cranial nerves?
» July 16, 2024: a potential breakthrough on facial pain as I have a most likely diagnosis of "Eagle Syndrome", believe it or not after referral by my dentist!. Eagle's syndrome is a condition associated with the elongation of the styloid process or calcification of the stylohyoid ligament. Eagle Syndrome (also called Stylohyoid Syndrome) is caused by an elongated styloid process and/or calcified stylohyoid ligaments and could explain pretty much all my eye/head/face issues as it effects the cranial / vagus nerves and carotid arteries. The vagus is the longest cranial nerve and comprises both sensory and motor fibers. the vagus nerve functions contribute to the autonomic nervous system, which consists of the parasympathetic and sympathetic parts. Carotid-type Eagle syndrome involves compression of the carotid sheath, with pain in the eyes and visual disturbance being common. I am undergoing physiotherapy by a specialized head physiotherapist.
» August 02, 2024: I cancel the physiotherapy for Eagle Syndrome as I judge it counterproductive. After three weeks of physiotherapy I have increased pain and significantly more worrisome facial events such as nerve strikes. Maybe my CIDP cannot tolerate the movement. One such strike, August 04, 2024, causing severe pain in my left cheek then eye for several seconds.
» August 13, 2024: Doctor - a Dental Surgeon - confirms I have an elongated styloid process and possible calcified stylohyoid ligament. See panoramic x-ray showing my elongated styloid process Laser treatment for the Eagle Syndrome ES is suggested but I on reflection will reject the laser for pain approach as I suspect it will worsen my CIDP. The ES Dental Surgeon doctor himself question how much of my head & face symptoms are caused by Eagle Syndrome versus my CIDP?
» September 03, 2024: I decided to resume taking oxcarbazepine at very low dose of 100 mg per day, as I discovered it is also useful in the treatment of Eagle Syndrome. (I last took oxcarbazepine in October 2021 for a year to treat my mini-seizures), The drug also seemed then to dampen my fasciculations that act to amplify pain. BIG QUESTION: Does Eagle Syndrome cause mini-seizures, arrhythmia, and both eyeball fasciculations, fasciculations generally and most of my facial pain. And what about the really weird spontaneous jaw-snapping I logged on January 12, 2021: How will we determine CIDP versus Eagle Syndrome / elongated styloid causation?.
» September 12, 2024: I feel oxcarbazepine is helping even at the very low dose. In February 2022 I was taking 600 mg per day for my mini-seizures. I decide to increase the dose from 150 mg to 225 mg per day.
» October 02, 2024: An appointment with a key neurologist is fruitless when he tells me he did not know what Eagle Syndrome / elongated Styloid is and will write the Dental Surgeon and tell him so! This is even though some of the symptoms he investigated could be caused by the syndrome. I am stunned as the Dental Surgeon was trying to take a multi-disciplinary approach with other doctors. Shockingly, I am beginning to think I have a big problem in getting the help I urgently need in Canada.
v My CIDP 2025 Getting Worse but No Resolution
» February 24, 2025: Hard to believe but I still have not been able to see a Eagle Syndrome specialist in Canada. On top of this I have myself discovered myself that the CT scan of my brain & neck March 02, 2021* on my ER visit clearly shows my right-side elongated styloid process - see CT scan image at this link.! My main highly esteemed well known CIDP specialist at the same hospital wrongfully referred to that scan as "normal" and wrote in a clinical note June 29, 2021: "Despite the normal brain and spinal CT scan done in March 2021, the patient still thinks that he needs to have a brain MRI as he reports some episodes of near syncope, but no typical syncope”. February 17, 2025 I wrote the ER Administration about the omission as well as the Radiologist-in-Chief of the Joint Department of Medical Imaging (JDMI) at the Toronto University Health Network!
» May 11, 2025: So four years later I am to have a neck CTA with contrast which should have determined the seriousness of my Eagle Syndrome, but it did not because it focused on arteries to the exclusion of veins. The scan did provide my right-side styloid process length at 4.1 cm which is considered elongated over 3 cm. The CTA is not able to detect cranial nerve issues. Apparently, nerves are not visible by normal scans, but the FIESTA MRI or neurogram are specifically designed to look at them. Meantime I am beginning to think that I have CIDP progression with related increased issues everywhere, especially limbs, as well as my facial cranial nerves.
» July 07, 2025: My Canadian ENT doc is not able to do anything further, such as a referral to a ES neurology specialist or order an MRI (FIESTA) to examine the cranial nerves. I am left hanging with apparently no concern by my doctors despite my concern for ongoing worrying issues such as with swallowing and breathing,
» July 09, 2025: I consult a US top specialist in Eagle Syndrome, an otolaryngologist, in an attempt to figure out the CIDP versus Eagle Syndrome causation issues. He says I have moderately thickened styloid process bilaterally and a close juxtaposition right greater than left against the transverse process of C1 †† On both sides the jugular vein tapers and essentially disappears around the level of the transverse process of C1. Surgical intervention is considered but he too is uncertain of outcome due partly to the causation issue of Eagle Syndrome versus CIDP.
» July 27, 2025: With my now significant study of Eagle Syndrome, I have become increasingly worried that many of the symptoms I have long thought of (and been told by some neurologists) are likely caused by CIDP, actually are triggered by my Eagle Syndrome. My CIDP doctors should have at least known about Eagle Syndrome as it seems I had cranial nerve issues from the outset (2011). Now I am trying to find a cranial nerve specialist who can tell me the extent to which the cranial nerves are demyelinated (by CIDP) and which are damaged or compressed by the styloid process (which would be Eagle Syndrome)
August 19, 2025: A viewer of my 2025 CTA tells me "Both IJVs look jammed between styloids and C1. Which means your vagus nerves are likely compress between IJVs and C1". This reinforces my belief that at least some of my major symptoms are caused by neurological vagus nerve issues.
September 15, 2025: I consult another US Eagle Syndrome specialist on whether I should have stylectomy / styloidectomy for my situation: He leans towards yes but leaves it up to me to decide. He counsels that ES is progressive and as you get older veins, arteries, deteriorate and dangers (of a stroke for example) increase. Both the ES specialists do not think it worthwhile to do a FIESTA MRI to investigate cranial nerves.
September 16, 2025: I am in a quandary on whether I should have a stylectomy (in the US) but feel I should decide sooner than later. I am attempting September 16, 2025 to get an urgent consult with my Canadian CIDP specialist as to causation of my cranial symptoms.
October 03, 2025: I would like to avoid the stylectomy but I have had a few pretty bad days lately. My headaches every day - Intercranial Hypertension? - alone is quite worrying as I told my family doctor this cannot continue without something even more disastrous occurring.
» October 24, 2025: Today a serious instance of swallowing difficulty. Last night a sudden breathing issue and earlier in the day an arrhythmia attack. All potentially cranial nerve issues from CIDP or Eagle Syndrome. Both legs also demonstrating deep (ligament) issues of weakness and pain caused by CIDP.
» December 15, 2025: Appointment with my CIDP doctor is depressing. Nerve Conduction Studies NCS confirm I am worse and talk of me ending in a wheelchair next year 2026 prevails. Still no treatment options (such as Rituximab) as new blood tests are negative for nodal antibodies. Despite having an SVT attack (with heart rate hitting 180 bpm plus a bodily tremor) during the consultation, cranial issues were not discussed and indeed the official clinical note reported my "cranial nerves are normal". (The heart doctors I have consulted advised me on multiple occasions that the trigger of my SVT is likely by the vagus nerve, which is cranial nerve 10).
v My CIDP 2026 Big Challenges with No Treatments
» January 20, 2026: I am in a quandary with no options available for relief from CIDP progression. I could go for the Eagle Syndrome styloidectomy potentially offering some cranial issues relief - but I am not convinced.
..
Also see:
> My CIDP Since Going-Solo without CIDP Drugs February 18, 2021 - July 16, 2024
> Summary IgG Infusions Log Pre-February 2021
† Cranial Neuropathy in CIDP-2021-01-01.pdf "Cranial nerves are infrequently involved in typical CIDP, but involvement is more common in multifocal acquired demyelinating sensory and motor neuropathy (about 50%). The facial nerve is the most commonly affected cranial nerve, often bilateral. Cranial nerve palsy was found in only 11% of both typical CIDP and DADS but was present in 48% of MADSAM patients. My CIDP is classified as MADSAM. "Of 31 patients with MADSAM, five had bulbar palsy with involvement of cranial nerves IX and X, of which four were bilateral; four had facial palsy, which was bilateral in one; three each had a III or VI nerve palsy; two each had a V or VIII nerve palsy"; "Bulbar palsy" refers to a condition characterized by problems with the function of cranial nerves IX (glossopharyngeal), X (vagus), XI (accessory), and XII (hypoglossal), which control muscles involved in speech, swallowing, and facial movement. For detail view:
4 Above as described in "Eagle-Syndrome-Key-Article-Westbrook-2020.pdf": Eagle’s syndrome, elongated styloid process and new evidence for per-manipulative precautions for potential cervical arterial dysfunction, and Cranial nerve involvement in typical and atypical chronic inflammatory demyelinating polyneuropathie-2020-08-26
See the 12 cranial nerves-2023-12-21 for a description.*
†† The transverse process of the first cervical vertebra (C1), also known as the atlas, is a bony projection that extends laterally from each of its lateral masses. These processes are crucial for providing attachment points for neck muscles and for housing the foramen transversarium, a canal that allows passage of the vertebral artery and vein
qqqq
Eagle’s syndrome, categorized initially by Dr. Watt Eagle, divides patients into two groups based on the structures compressed or irritated by the styloid complex. The classic form involves cranial nerves 5-tri geminal, 7-facial, 9-glossopharyngeal, and/or 10-vagus, and the vascular form involves the internal carotid artery (ICA), external carotid artery (ECA) (Eagle, 1948), periarterial sympathetic nerve plexus (Eagle, 1949), and more recently in the literature, the internal jugular vein (IJV) (Dashti et al., 2012).

Click for larger view of above image: Eagle-Syndrome-explained-Westbrook-2023
There are four forms of Eagle Syndrome:
- Neuropathic Eagle Syndrome (NES) - or Classic Eagle Syndrome
- Carotid Eagle Syndrome (CES)
- Jugular Eagle Syndrome (JES)
- Compass Eagle Syndrome (CoES)
†† Is Eagle Jugular Syndrome an Underestimated Potentially Life-Threatening Disease? In conclusion, we think that, amongst others, Eagle syndrome may result in compression and thrombosis of the jugular vein, thus causing life-threatening clinical manifestations, including cerebral venous thrombosis, as reported by Fu-Liang Zhang et al.,1 along with isolated, recurrent, pulmonary embolism events, the origin of which may be misdiagnosed. The dynamic exploration of the spatial relationship between elongated SPs and jugular veins though CTA and/or MRA may lead to a prompt diagnosis of this eventuality and to an effective treatment of these patients. Further investigations are needed to confirm or deny our hypothesis.
May 6, 2024: "One case of sudden death due to Eagle syndrome is also reported, caused by the mechanical irritation of the carotid sinus by an elongated styloid process with consequent acute cardiovascular failure"
"* The gold standard for Eagle Syndrome imaging is a dynamic CTA scan with contrast and/or MRA.*Apophysis is a secondary ossification center that fuses with the bone over time and attaches tendons or ligaments. Elongation of the styloid apophysis* may give rise to intense facial pain, headache, dysphagia, otalgia, buzzing sensations, and trismus. Apparently, nerves are not visible by normal scans, but the FIESTA MRI or neurogram are specifically designed to look at nerves. The latter may be what I will need due to cranial nerve issues..
See other Eagle Syndrome references in "My Message to Doctors"
Concepts for My CIDP log of CIDP versus Eagle Syndrome 2024: Eagle Syndrome, Stylohoid Syndrome, Stylalgia, calcified, styloid, ligament, tendon,ossification, Neuropathic Eagle Syndrome NES or Classic Eagle Syndrome Carotid Eagle Syndrome CES CIDP pedagogic hallucination vagus nerve (VN), the principal component of the parasympathetic nervous system cidp mimicks Canada Eagle Syndrom ES doctors Dental Department Sunnybrook Hospital Toronto Canada
