My Breathing-Respiratory Issues are CAUSED by CIDP?
- experts disagree =>
My breathing issue became serious in early 2012 when I started having a few breathing seizures mostly diaphragm-centered and one critical when my windpipe "collapsed" for about one minute. At first I could not believe that this was CIDP at work. Indeed my one very good CIDP specialist doctor says that my breathing issues are not caused by CIDP; while the other said my breathing issue was not life threatening (but prescribed IVIG anyway)! Now for me though it is more "clear" that CIDP has indeed caused my breathing problems and it seems all the muscles in my abdomen have been affected (fasciculations, loss of control, cramping and weakness). Even if my doctors were right on this breathing issue, there is very strong evidence that the IVIG treatment I had in 2013, 2015, and now again 2016 had a dramatic positive effect in stopping the most serious problems I had with my breathing (such as major events of 'stop breathing'). My breathing issues as at June 2015 are described below -
| Description of my Breathing / Respiratory Symptoms | ||||||
| Severity* | Symptom Complaint | |||||
| Rank | Weight | Title | Symptom Description | |||
| 1 | 6.0 | Breathing Issue | Complex issue of a heavy diaphragm feel, "reset" gasping events, real & imaginary stop breathing, and diaphragm / chest / abdominal muscle or nerve pain | |||
| 1.1 | 2.0 | gasping events | Sudden involuntary breathing "reset": during normal breathing an inexplicable involuntary catch-breath inhale or exhale ("breathing-hiccup") episodes. Gasping episodes occurring while awake in normal activities whether active or relaxing. In extreme case breathing-seizure event ("respiratory arrest") of windpipe or diaphragm muscles | |||
| 1.2 | 1.0 | running | Sudden difficulty breathing episode or event when running long distance 8.5-10km at pace that was without any effort or elevated breathing prior to CIDP. Occurs at slow speed too brought on by jerk or twist. | |||
| 1.3 | 2.0 | punched-in-stomach | Feeling of being punched in the stomach and winded causing breathing tightness and central chest pain. Sore diaphragm. Weakness in whole abdominal area, yet muscles feeling solid. | |||
| 1.4 | 1.0 | diaphragm pain | Peculiar acute pain occurring particularly in left-side diaphragm muscle directly at rib-cage. Diaphragm tightness and pain. | |||
I have abdominal weakness, digestive discomfort, swallowing, voice and general neck issues which seem to relate to the ventilatory issues. Indeed sometimes the problems are in a combined event lasting from seconds to hours.
![]() FINALLY - September 22, 2015 a Respiratory Specialist found I do indeed have one abnormal respiratory test, to quote: the "patient had MIPS and MEPS done in the Pulmonary Function Lab today, both of which are significantly reduced, particularly the MIPS. This confirms that he has a neuromuscular syndrome affecting the diaphragm".
FINALLY - September 22, 2015 a Respiratory Specialist found I do indeed have one abnormal respiratory test, to quote: the "patient had MIPS and MEPS done in the Pulmonary Function Lab today, both of which are significantly reduced, particularly the MIPS. This confirms that he has a neuromuscular syndrome affecting the diaphragm". 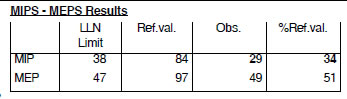 The MIP = 34% of normal (Max Inspiratory Pressure) reflects the strength of the diaphragm and other inspiratory muscles, while the MEP = 51% of normal (Max Expiratory Pressure) reflects the strength of the abdominal muscles and other expiratory muscles. However, my CIDP specialist doctor November 24, 2015 says she does not accept this view insisting that CIDP is not the cause? As the breathing issue investigation continued I had a gene test for Pompe Disease which disease admittedly causes symptoms similar to mine. Pompe Disease results from a mutation of the acid alpha-glucosidase gene (GAA) gene. The test was negative for Pompe. See above right table showing my MIP and MEP results with pressure in units of cm-water. Meantime December 2015 through February 2016 I took a IVIG break (as it was wearing me down).
The MIP = 34% of normal (Max Inspiratory Pressure) reflects the strength of the diaphragm and other inspiratory muscles, while the MEP = 51% of normal (Max Expiratory Pressure) reflects the strength of the abdominal muscles and other expiratory muscles. However, my CIDP specialist doctor November 24, 2015 says she does not accept this view insisting that CIDP is not the cause? As the breathing issue investigation continued I had a gene test for Pompe Disease which disease admittedly causes symptoms similar to mine. Pompe Disease results from a mutation of the acid alpha-glucosidase gene (GAA) gene. The test was negative for Pompe. See above right table showing my MIP and MEP results with pressure in units of cm-water. Meantime December 2015 through February 2016 I took a IVIG break (as it was wearing me down).
> Getting Worse: February 2, 2016 follow-up breathing tests indicate a further weakening of my diaphragm (MIP dropped from 34% to 27%) and other expiratory muscles (No IVIG for three months previously). > Improvement July 26, 2016: Today good news, my MEP hit 90% and MIP 60% - clearly still serious but a major positive reversal in direction! (Taken after four months of maintenance dose IVIG immunoglobulin). My respirologist tells me that diaphragm muscles take time to repair after nerve damage although he cannot guarantee a full recovery to 100% MIPS & MEPS. A huge relief and I am indeed hopeful as I expect my running will provide the exercise to get me back! The respirologist tells me that breathing itself is really the best and only good exercise for the diaphragm.
Nevertheless, my very expert CIDP specialist doctor is categoric that my breathing issues are not related to CIDP. This is despite the fact that my breathing symptoms dissipate with IVIG infusion treatment! During IVIG I did not have a single major breathing event (breathing seizure) and even my breathing hiccup episodes almost totally stop! In addition, my February 2, 2016 further weakening of my diaphragm muscles could be attributed to the IVIG holiday I have had last two months. In the last few weeks, since I paused IVIG to this date, I have also experienced the gradual return of breathing hiccup episodes. Back on IVIG for four months hiccups subside and MIPS/MEPS diaphragm strength July 26, 2016 show MAJOR improvement! The situation I am in is confusing and quite troubling to me: Without an explanation I cannot be entirely persuaded by my CIDP doctors that CIDP was not the cause of my breathing issue, despite my huge respect for their capabilities.
However, what I can say with a high level of confidence: as of now, December 2017 the breathing issue that began in 2012 as a life threatening issue is now no more. I believe it has almost totally resolved - only a few hiccups (breathing rhythm reset) no real breathing difficulties. I predict upcoming breathing tests early 2018 will show close to normal MIPS and MEPS (Let us see if I am right!). . .
> I was right: Recovery Complete : January 23, 2018 follow-up breathing tests show MIPS and MEPS normal range - MIPS at 76% of predicted and MEPS at an astounding 140%! No further follow-up required. This history is well illustrated in my CIDP Breathing Index shown below -.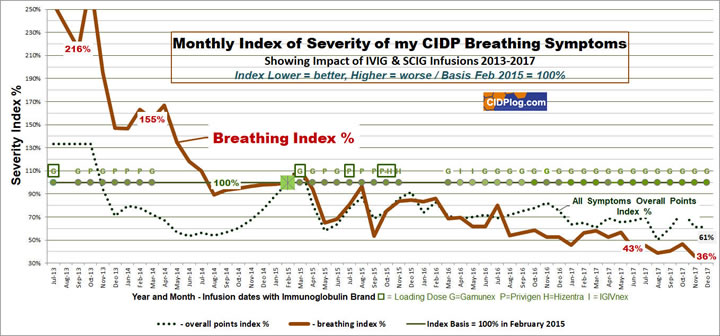
> View Larger Breathing Index Chart in PDF
Prior to September 2015, and for a number of years, repeated standard breathing tests were normal but I get frequent breathing-hiccups, my diaphragm seizes-up without apparent reason and sometimes when I run! These breathing incidents are clearly NOT normal leading me to question the method & reporting for the breathing test carried out at two leading pulmonary function laboratories. I had some difficulty carrying out the breathing actions for the test but this difficulty was not even reported : but something was wrong and I do not think they would detect the problem I have - "breathing interruptions" while shortness of breath is secondary to this main issue of interruptions. I have had cardiac (including catheterization angiogram) and MRI investigations (of heart, organs and abdomen) with no issues. Also I do not think even now in February 2016 that my neurologist is placing sufficient priority on my breathing issue: In particular I believe I may be at risk as I am only (as of February 26, 2016) on a low maintenance dose IVIG and this may not be sufficient to control my respiratory problems. Now August 2016 I do feel I am recovering quite well from this breathing issue: My own "breathing index" (chart shown above) has reached a three-year low of 51% and I am managing to run 10km with very little breathing discomfort. I am hopeful!
My current feeling is that CIDP is indeed directly (by nerve damage) and/or indirectly the cause of my breathing problems. By "indirectly cause" I theorize that the extreme tightness, cramping tendency, and fasciculations in my abdomen-and-neck, including diaphragm cramping, somehow interferes with my breathing. CIDP is considered the chronic form of Guillain-Barre Syndrome GBS where breathing issues are a recognized symptom and I wonder if CIDP should be excluded as the cause of by breathing condition in this fashion. See John Hopkins Medical Centre treats Guillain-Barre (/ CIDP?) patients with such breathing conditions - including "weakness of their breathing and difficulty chewing and swallowing"!
> March 2020 COVID-19 Coronavirus Pandemic : Since my last post two years ago I have only had a couple of breathing events and also the occasional breathing hiccup. But now in March 2020 we face the troubling COVID-19 Coronavirus Pandemic that, speaking frankly, would kill me if contracted. Covid-19 is a respiratory virus. But on the contrary, I found IVIG helped with my respiratory problem and interestingly and starting late March 2020 some trials are indicating high-dose IVIG is an effective treatment for late-stage Covid-19 patients! Mid-April 2020 Octapharma (who make Panzyga IVIG and Cutaquig SCIG bands) are starting trials as I write. Is there some extraneous effect at work that IVIG helps with breathing generally? Nevertheless, covid-19 is a severe acute respiratory syndrome and I am worried: I started another page to log my management of Covid-19 with CIDP. See CIDPlog COVID-19.
> CIDP Breathing October 11, 2021: Since February 2021 I have been off all drugs and now have some strange breathing issues. I have breathing hiccups (like a reset) almost every day but these are not severe. I think my autonomic breathing is sometimes too shallow or two slow and get this involuntary reaction. Also I feel faint or dizzy sometimes which may be due to shallow breathing: I am increasingly resorting to taking a few deep breaths when I feel dizzy and this may be helping with this breathing issue. At night, I have had some stop-breathing events (sleep apnea?) and sometimes have to shake my head to recover from a fuzzy brain sensation. So into mid-2022 I seem to have some kind of uncomfortable chronic breathing issue with an uncertain horizon.
> CIDP Breathing Turns Critical January 17, 2023: Last night I faced a near-death breathing crisis waking me up from a deep night sleep. Doubly worrying as I had the same three-days ago when I was taking a day-time nap. Actually I did have such an event about a month ago but I had hoped that this type of attack would be a one-off and also a day-time thing while napping on my back. I was sleeping on my side this last time and truly found it horrifying. I seemed to have no control over the recovery process. Following the attack I just took the plunge and risked going straight back to sleep with no further complications. Analyzing this, I remember yesterday feeling my breathing felt strained.
Please write me with your CIDP experience: I would like to hear from CIDP patients who have had breathing issues. My email address editor@cidplog.com
There are expert articles that seem to suggest that CIDP breathing issues can develop (in particular when there is phrenic nerve involvement or damage (phrenic nerve palsy). Some examples are -
"Chronic inflammatory demyelinating polyneuropathy and ventilator failure: report of seven new cases and review of the literature" Published 2011
S A Zivković, A C Peltier, T Iacob, D Lacomis. Acta Neurologica Scandinavica 07/2011; 124(1):59-63. DOI:10.1111/j.1600-0404.2010.01431.x · 2.44 Impact Factor
ABSTRACT: Ventilatory involvement is rarely reported in chronic inflammatory demyelinating polyneuropathy (CIDP), but small prospective studies showed frequent involvement of phrenic nerves, which is usually overshadowed by severe limb weakness. To report the clinical features of CIDP associated with ventilatory failure. There were seven patients (43% women), with a mean age of 58.6 (range 38-82). The clinical courses were relapsing in five and progressive in two. Four patients had an initial event simulating Guillain-Barre syndrome (GBS). Ventilatory failure was recurrent in three patients. Five patients had full or nearly complete recoveries; one still requires nocturnal ventilation; and one died (14%) of myocardial infarction while still requiring mechanical ventilation. Clinical ventilatory dysfunction in CIDP is usually not an indicator of poor prognosis, and many patients recover without significant permanent disability. The mortality rate is similar to intubated patients with GBS. Patients with cardiopulmonary comorbidities and acute GBS-like onset of CIDP may be at higher risk of ventilatory failure which typically responds to 'standard' treatments of CIDP. Larger prospective studies are needed to define the prevalence, clinical spectrum and significance of ventilatory involvement in CIDP and to establish guidelines for evaluation and treatment. Chronic inflammatory demyelinating polyneuropathy, phrenic nerve and respiratory symptoms.
"Unusual features in chronic inflammatory demyelinating polyneuropathy: Good outcome after prolonged ventilatory support" Published 2011
Sanjeev Jha, MK Ansari, KK Sonkar, and VK Paliwal. J Neurosci Rural Pract. 2011 Jul-Dec; 2(2): 171–173.
ABSTRACT: Severe respiratory muscle paralysis and ventilatory failure is rare in chronic inflammatory demyelinating polyneuropathy (CIDP). We report a 14 year child who presented with respiratory failure, bulbar and multiple cranial nerves involvement along with bilateral phrenic nerve paralysis. He was diagnosed with CIDP after electrophysiological evaluation. He required AMBU ventilation for about 4 months (including domiciliary use), after which he recovered significantly. Along with several unusual features of CIDP, this report highlights good example of steady basic intensive care to save lives and rewarding outcome of prolonged respiratory support, provided by AMBU ventilation which is a rather primitive, but inexpensive device.
"Chronic inflammatory demyelinating polyneuropathy and respiratory failure due to phrenic nerve involvement" Published 2010
Cengiz Tataroglu, Ayca Ozkul, Ahmet Sair. Journal of clinical neuromuscular disease 09/2010; 12(1):42-6. DOI:10.1097/CND.0b013e3181d80bdc
ABSTRACT: In this article, 2 patients with chronic inflammatory demyelinating polyneuropathy (CIDP) are presented. These patients developed respiratory failure which could not be explained by any cardiac or pulmonary pathology. The first case had pure motor involvement and probable CIDP, and the second case had severe sensorial dysfunction and an ataxic picture in addition to motor symptoms. His clinical picture was compatible with distal acquired demyelinating sensory neuropathy without M protein. Electrophysiologic investigations of both patients disclosed impaired phrenic nerve conduction and neurogenic motor unit changes in the diaphragm. Both patients showed a moderate response to immunotherapy. Distal acquired demyelinating sensory and pure motor variant of CIDP can be a cause of respiratory dysfunction. Different clinical patterns of CIDP should be evaluated for phrenic nerve involvement. Chronic inflammatory demyelinating polyneuropathy, phrenic nerve and respiratory symptoms. In conclusion, phrenic nerve involvement should always be considered in CIDP patients with respiratory failure, and clinicians should always be aware of phrenic nerve involvement in different CIDP variants. Respiratory failure in the pure motor variant of CIDP and DADS may be due to phrenic nerve involvement, which shows a moderate response to immune therapies. Neurophysiologic evaluation of the phrenic nerve and pulmonary functional tests in different subgroups of CIDP may clarify the pathogenesis and hence help to prevent the more severe features of respiratory failure.
"Chronic inflammatory demyelinating polyneuropathy, phrenic nerve and respiratory symptoms" Published 2005
João Costa University of Lisbon, Lisbon, Mamede de carvalho Faculty of Medicine- Universit... Neurology
Department of Neurology, Hospital de Santa Maria, Lisbon, Portugal. European Journal of Neurology (Impact Factor: 3.85). 02/2005; 12(1):64-6. DOI: 10.1111/j.1468-1331.2004.00961.x Source: PubMed
ABSTRACT Respiratory involvement in chronic inflammatory demyelinating polyneuropathy (CIDP) has been very recently described. Phrenic nerve conduction studies have been described as useful to detect respiratory impairment in these patients. This study describes two patients with CIDP, in whom neurophysiological studies of the respiratory muscles were performed. The first patient had severe respiratory insufficiency, and phrenic nerve studies disclosed no motor responses and electromyography (EMG) of the diaphragm confirmed severe loss of motor units, bilaterally. On treatment, we documented clinical and neurophysiological improvement. In the second patient, phrenic nerve studies showed abnormal results; however, EMG of the diaphragm ruled out loss of motor units. The first case represents the risk of phrenic nerve involvement in this disorder, and the potential recovery on treatment. The second case illustrates that the temporal dispersion of the motor responses can be misleading, and EMG of diaphragm should be performed to confirm the loss of motor units.
CONCEPTS for My Breathing Issues are CAUSED by CIDP: breathing, CIDP shortness of breath, immunoglobulin, Dyspnea uncomfortable abnormal awareness of breathing, respiratory arrest, CIDP respiratory distress, digestion, cardiac, autonomic, neuropathy, phrenic nerve involvement in CIDP, breathing-seizure ("respiratory arrest") of windpipe or diaphragm muscles, AMBU ventilation, bulbar palsy, chronic inflammatory demyelinating polyneuropathy, phrenic nerve palsy, Parsonage-Turner syndrome (PTS), conduction studies or electromyography, COPD, chronic obstructive pulmonary disease, covid-19 cororavirus pandmic,
